We’re Moving our Provider Portal to Availity Essentials™
| To make it easier for providers to self-service, we’re moving our provider portal to the Availity Essentials™ platform. The final move will happen in early 2026. At that time the AZ Blue provider portal will close. For more information about the portal transition, see our provider FAQs. |
It’s easy. To register for Availity Essentials, choose an administrator to activate your account and then follow the process outlined on availity.com/azblue.
Once your account is set up, your administrator can create user accounts for your staff.
Here’s what we like about Availity Essentials:
- Real-time access to multiple payers – You can save time by working with AZ Blue and other payers on a single platform.
- User-friendly experience – Many of the workflows integrate with each other, making it easy and efficient to navigate to the next step in your process.
- Best practice capabilities – Provider feedback, industry-standard technology, and extensive research help Availity’s platform stay reliable and on the cutting edge.
- Comprehensive user support – You’ll find “help topic” info buttons throughout the portal. Simply click for quick support. On-demand demos walk you through the “how to” right when you need it. Availity offers free webinars and you can message or call the Availity support team with portal questions: 800-282-4548.
AZ Blue is currently set up on the Availity Essentials portal with the following features:
- Eligibility and benefits inquiry
- Claim submission (professional, facility, dental)
- Claim status (includes three "quick search" tabs)
- Remittance viewer
- Fee schedules (for contracted providers only)
- EFT (new enrollments or changes)
- AZ Blue “payer space” for links to additional AZ Blue resources
- Coming in early 2026: Prior auth requests and status dashboard
- Coming in early 2026: Claim attachments (submit records with your claims or from the Availity claim status dashboard)
- Coming later in 2026: Claim appeals (initiate a claim dispute from the claim status dashboard)
- You can only use the AZ Blue provider portal until our move to Availity Essentials is complete and the AZ Blue provider portal is sunset in early 2026.
Note: Our Availity “Payer Space” makes it quick and easy to access AZ Blue tools and content from within the Essentials workspace. - Yes. We're building it out with features such as prior authorization, claim attachments, and claim appeals. We will also continue to enhance previously implemented functionalities.
Availity makes it easy to navigate, search, and access “how to” information right from the portal homepage. You’ll see strategically placed “help topic” buttons that guide your experience.
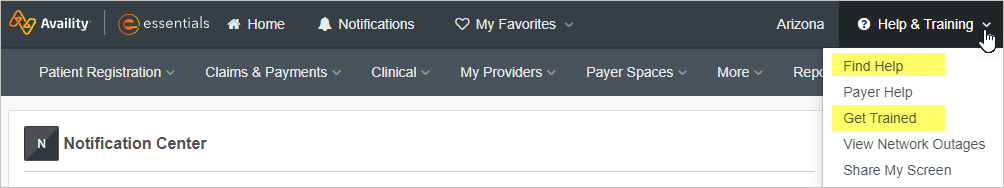
Look for free webinars and on-demand training resources via the Help & Training dropdown menu in the dark gray menu bar:
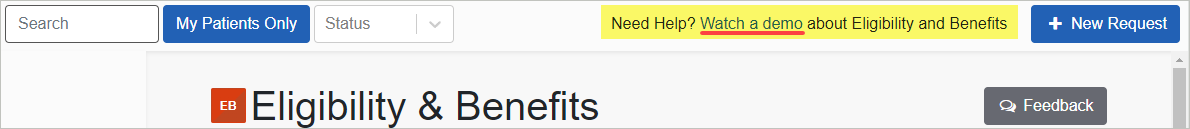
Availity posts a recorded demo in each feature to demonstrate how things work. You’ll find the demo links near the top of the page, as shown here in the Eligibility & Benefits screen:
You can also message or call the Availity customer service team with questions: 800-282-4548.
Most plans are supported through Availity Essentials, including:
- Most employer group plans (with various AZ Blue prefixes).
- Individual/ family plans (with prefixes EPI, FLH, FQL, IPO, NNG, and NNJ) - One exception is the "ACA Standard Health with Health Choice" plan (prefix IAZ), which is administered by our ACA Health Choice team at azblue.com/aca-standardhealth-health-choice.
- Federal Employee Program® (FEP®) plans (prefix R) – Supported on the portal except for member ID cards and benefit books (see FEP Plan Brochures).
- BlueCard out-of-area plans from other Blue Plans (with various non-AZ Blue prefixes) – Supported on the portal except for member ID cards and benefit books.
- Medicare Advantage PPO plans from other Blue Plans (with various non-AZ Blue prefixes) - Supported on the portal except for member ID cards and benefit books.
- Medicare Advantage HMO plans administered by AZ Blue (prefix M2K) – For all of our Medicare Advantage plans, you can access member eligibility and benefits via the Availity Essentials portal. For prior authorization and claim/payment services, check the back of the member ID card for the plan administrator. You can use the Availity portal for the plans administered by AZ Blue. The other administrators have their own provider portals: Arizona Priority Care (AZPC) and Optum Health Network Arizona (OHNAZ).
- Medicare Supplement plans (prefix XBS).
Certain plans are only partially supported through Essentials: Click here for details.
If you have questions about how to register for the Availity Essentials portal, please review the Availity Essentials Registration Training site.
If you have other questions or need more help, call Availity Client Services at 800-AVAILITY (282-4548). You can reach them Monday through Friday from 8 a.m. to 8 p.m. Eastern Time (excluding holidays).
Availity is a separate, independent company contracted with AZ Blue to provide website portal services for the providers who care for our members. Availity is a registered trademark and Availity Essentials is a service mark of Availity, LLC.
Optum Health Network of Arizona (OHNAZ) is a separate, wholly owned subsidiary of Optum and is contracted with AZ Blue to provide utilization management and claim/payment processing services for providers and attributed members in Maricopa and Pinal counties with AZ Blue Medicare Advantage HMO plans.
Arizona Priority Care (AZPC) is a separate, independent company contracted with AZ Blue to provide utilization management and claim/payment processing services for providers and attributed members in Maricopa and Pinal counties with AZ Blue Medicare Advantage HMO plans.
Blue Cross, Blue Shield, the Cross and Shield Symbols, Federal Employee Program, and FEP are registered service marks of the Blue Cross Blue Shield Association, an association of independent Blue Cross and Blue Shield Plans.